Hey there. I’ve been dealing with some dizziness/balance issues for about 7 years. I’ve had extensive work ups with a number of different physicians. A couple of them (my primary, 2 ENTs, and a neurologist) said their best guess was MAV. Can someone tell me if my symptoms and history track with what you are experiencing?
History
I’m a 37 year old male. Healthy BMI. Very physically active. Moderate drinker. Non-smoker. Onset of symptoms at approximately age 30. Family history of migraine (father and aunt). Symptoms developed slowly. Currently, they are stable (new episodes are not worse than prior episodes) with exacerbations in frequency that can last weeks or months at a time. I have not experienced any head pain, only the symptoms listed below.
Symptoms
Balance/Dizziness:
- Episodic, difficult to describe, non-vertiginous imbalance. Episodes typically begin within an hour or two of waking up in the morning and last 2 to 8 hours. It feels like I’ve been drinking when I’m completely sober. This imbalance does not seem to be noticeable to those around me. It worsens with standing and walking and improves to the point of being almost negligible with lying down. Episodes resolve toward late afternoon or evening, but with some mild, lingering symptoms.
- Two brief (minutes long) episodes of rotational vertigo, both woke me from sleep in the middle of the night and caused me to fall out of bed. Only two episodes since beginning of symptom onset 7 years ago, though. These two episodes were preceded by vivid, disturbing dreams. This is not a prominent feature.
- A handful of minor falls (not drop attacks) that I attribute to my impaired sense of balance.
- Mild, persistent balance disturbance experienced almost constantly with very brief periods of what feels like total remission on some days.
Ears:
- One or two incidents a year of middle ear clogging with bulging ear drum and visible fluid. No such symptoms in the last year or so.
- Severe, sensorineural hearing loss in the high frequency range in the right ear (not Meniere’s).
Cognitive/Emotional:
- Slowed thinking, absentmindedness, difficulty concentrating, difficulty finding words or remembering names, what feels like an overall drop in IQ coinciding with episodes of imbalance. Difficulty being productive during these periods.
- Heightened anxiety immediately after an episode resolves. Whereas I am slow (drunk feeling) during the episode, I am high strung (like I’ve had too much coffee) after an episode. Occasionally, this has felt less like anxiety and more like a full-blown episode of panic.
- Irritability and emotional lability that may precede episodes by a few days, but I’m not 100% certain of this connection. I am occasionally unreasonably irritable, and embarrassed by this after the fact.
Cardiac/Respiratory:
- Heart palpitations (PVCs). Unclear of temporal relationship to balance episodes. Listing here in the interest of being thorough. Timing of symptom onset (+/- age 30) coincides with timing of balance episodes. Overall, these improve/disappear during periods when balance symptoms also seem to be in remission, but the two do not always coincide.
- Periods of difficulty getting a satisfying breath. Need to yawn/sigh a lot. Feels like my diaphragm or rib cage don’t have room to adequately expand. Relationship to balance episodes unclear.
Digestive/urinary:
- Occasional constipation/bloating. Onset timing similar to other symptoms. This was never a problem prior to age 30. Maybe unrelated. Again, being thorough. Abdominal bloating occasional feels moderate to severe.
- Occasional feeling that I’m not peeing as frequently as I should be or that I’m retaining water. Wedding ring doesn’t fit like it used to, too tight at times. Diuretics helped this but did not improve dizziness symptoms.
Sleep:
- Occasional hypnagogic hallucinations while falling asleep or immediately upon waking up. Typically (at least once a week), a brief (< 1 second) flashbulb type light that I see on the back of my eyelids right as I start to fall asleep. On maybe 3-4 occasions, auditory hallucinations upon awakening - typically a single word that sounds like a whisper and repeats for a few seconds.
- Frequent (sometimes every night for weeks) hypnic jerks at sleep onset. Often large muscle groups (hips, thighs, shoulder, ankle) with no apparent pattern.
- Vivid dreams or nightmares, although these have subsided as I’m not currently taking medication.
- Once a year, a night terror where I jump out of bed and run into the living room or do some other stupid thing only to come to my senses and not know what I’m doing there. These are more frequent when taking medications that impact the quality of my sleep. Again, probably not related to dizziness, but being thorough.
Medical Work Ups
Doctors Seen: 3 primary physicians, 2 ENTs, 2 neurologists, 2 cardiologists
Cardiac: No relevant structural or rhythmic findings despite full gamut of tests.
ENT: No peripheral vestibular problems and no permanent central findings. Both ENTs thought MAV was most likely as my dizziness seems to be central in origin and fluctuating in occurrence. Hearing loss evident on audiometry, as noted above. This is not well explained.
Neurology: No relevant findings on imaging or during neurological exam. Second neuro also thought MAV. Two EEGs negative for seizures.
Respiratory: Normal lung function.
Metabolic: Blood tests are fine. Liver enzymes fluctuate and are sometimes mildly elevated. Docs don’t think this is relevant.
Sleep: Two full polysomnographies that were unremarkable. One normal polysomnography the day before a bad day of symptoms. I think that rules out sleep disorder as their origin. One MSLT that revealed a single SOREM episode. Not enough for a narcolepsy diagnosis.
Overall: I have very good insurance, and I feel like I’ve had every test known to mankind over the last 7 years. Docs are like, “¯_(ツ)_/¯, maybe migraine?”
Factors Influencing Symptoms
Things that make me worse:
- Alcohol consumption doesn’t seem to cause an episode right away, but a serving or two of alcohol the night before can worsen both the severity and duration of symptoms the next day. Heavy drinking (4+ servings) results in a full day of symptoms that are more severe (but still not enough to keep me bed-ridden or anything).
- Visual noise can trigger an episode. Grocery and retail stores almost always result in an episode of varying intensity and duration, especially if visited early in the day. Visiting my kids’ school where there are posters on the walls and things hanging from the ceiling makes me feel uncomfortable. Birdwatching, where I’m trying to pick out an individual bird among the branches of a tree, can trigger an episode.
- Motion can cause problems, with some caveats. Cleaning the house (moving back and forth to put things away) can trigger an episode. Scrolling on a computer or on my phone can cause an episode. This is especially true if there is a lag on the browser and the motion of the browser that I expect is delayed by a second or two. Tree branches and tall grasses that sway in the wind cause me problems sometimes. I do not, however, have problems with crowds or motion intolerance due to driving. I used to sea kayak in the Atlantic, and I had more difficulty moving back and forth on land to gear up my kayak than I did being rocked up and down by waves in the ocean.
- Metoprolol made me way worse, both in the dizziness and cognitive symptoms. I found this interesting, as it is a common migraine prophylactic. I attribute the worsening of my symptoms with metoprolol to the way that it negatively impacted my sleep. Sedating medications in general make me feel worse.
Things that make me better:
- A nap can completely stop an episode. In fact, if I get a good nap during an episode (1 hour or more), I sometimes wake up feeling 100% symptom free.
- Lying down improves the balance symptoms.
- Regular exercise seems to reduce the frequency and severity of symptoms, although I find exercises where the ground scrolls beneath my feet (running outdoors, hiking, bike riding) uncomfortable. I am able to run on a treadmill and even rock climb without incident.
- I recently moved from the East Coast (lots of trees and irregular sunlight patterns shining through the trees) to the Great Plains (wide open spaces with regular sunlight) and my symptoms have improved.
- My symptoms are less frequent and severe during the summer than they are during the winter. I attribute this to lifestyle changes. I spend more time outdoors and I get more exercise in the summer. During the winter, I spend more time indoors, encounter more visual noise, and I spend more time on the computer.
- Time of day matters. I usually feel pretty good in the early to late evening.
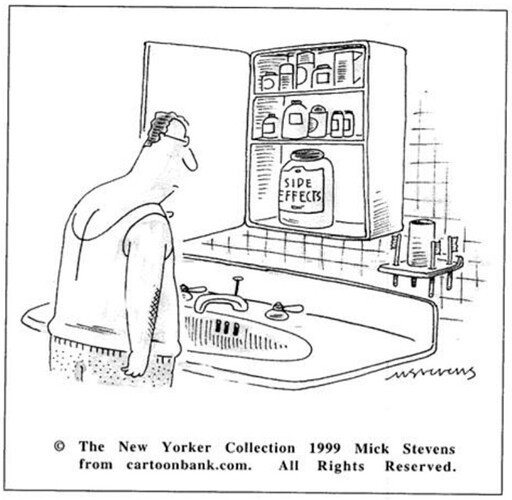
- I briefly experimented with buspirone and had some success. If I took a low dose twice a day, I felt worse. But if I took a single dose (only 5mg) at bedtime, I would feel almost symptom free the next day. It’s like the buspirone itself made me feel worse, but the rebound from the buspirone wearing off made me feel better. I didn’t continue this medication due to some side effects (tremors being the most bothersome).
I apologize for the length of this post. I’ve lurked on forums ever since I first started experiencing symptoms, and this is my first time to post anything. Can any of you tell me if this tracks with your experience? My primary care doc and the ENT that I’m currently seeing want me to experiment with a low dose of amitriptyline. I’m eager to feel better but anxious about trying a new medication. Any insight here is helpful.